|
 |
By Dr. Sina McCullough, Special to The MAHA Report
The release of the 2025–2030 Dietary Guidelines for Americans (DGA) marks a pivotal moment in our nation’s health journey. For the first time in decades, the conversation has officially shifted toward a concept we can all celebrate: ‘real food’– whole or minimally processed foods, according to the new guidelines.
Announced jointly by HHS Secretary Robert F. Kennedy Jr. and USDA Secretary Brooke L. Rollins on January 7, the guidelines take a bold stance against the industrial ultra-processed foods, added sugars, and industrial seed oils that have dominated our grocery aisles for forty years. This turn to ‘real food’ is a massive victory for anyone who believes that health begins with whole, natural ingredients.
But as with any major paradigm shift, policy change happens incrementally. While the new guidelines have successfully embraced the “Real Food” philosophy, they also allow us an opportunity to better understand saturated fats – specifically the role they have played and continue to play in supporting human health.
The Protein-Fat Balance: A New Opportunity
One of the most positive updates in the new guidelines is the encouragement of higher protein intake (1.2–1.6g per kg of body weight). This recognizes the vital role protein plays in metabolic health and longevity.
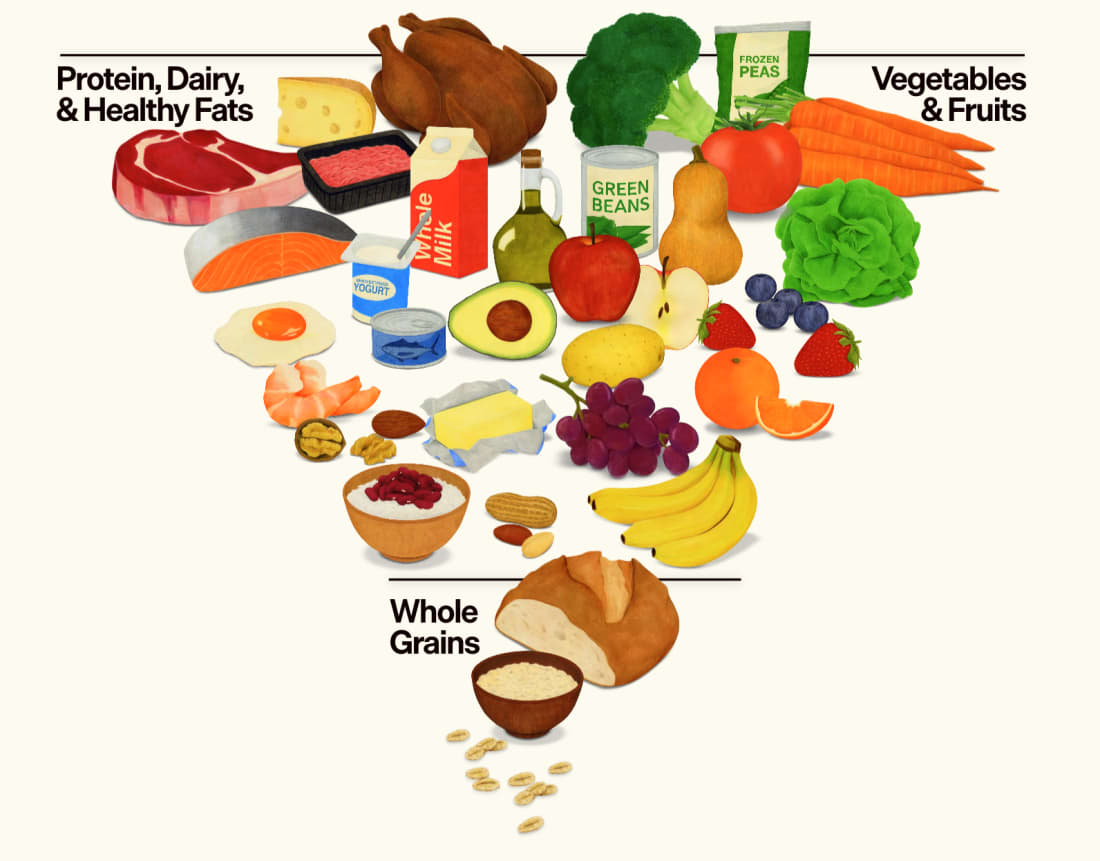
However, for those of us who love whole foods, this creates an interesting puzzle. Nature rarely isolates macronutrients. High-quality proteins, like eggs, beef, and whole milk, naturally come paired with saturated fats.
Under the current guidelines, which retain the traditional 10% cap on saturated fat, hitting these optimal protein targets with the recommended whole foods can be mathematically challenging. If you rely solely on the “10% rule,” you might need to lean toward egg whites instead of whole eggs or skinless poultry, missing out on the nutrient-dense matrix that nature provides.
But here is the good news: the health impact of saturated fat depends on what you eat with it. In the context of the Standard American Diet, such as a burger with a sugary soda and refined bun, high insulin levels stimulate the body to store the fat. But in a whole-food diet, stripped of those refined carbohydrates, the narrative changes. That same fat serves as energy and nourishment, delivered in a complex ‘food matrix’ alongside the vitamins and minerals nature intended.
The Root of the Fear: A 50-Year-Old Hypothesis
The 10% saturated fat cap is a relic from the 1950s that has become the bedrock of American nutrition policy.
It started with the “Lipid Hypothesis,” which posited that eating saturated fat (like butter and red meat) raises cholesterol, and that high cholesterol, in turn, causes heart disease. But the foundation of this theory was shockingly weak.
It was largely inspired by studies on rabbits, herbivores that were not designed to metabolize dietary cholesterol, and a single observational study by Dr. Ancel Keys known as the “Seven Countries Study.”
Keys’s study was deeply flawed. While he claimed to find a correlation between fat intake and heart disease, he “cherry-picked” his data. He purportedly had data from 22 countries but selected only the seven that fit his hypothesis, ignoring nations like France and West Germany where high fat intake did not correlate with high heart disease rates. Furthermore, his data from Greece was collected during Lent, when the population was abstaining from animal foods, creating a distorted picture of their true diet.
Even worse, while the study included 12,763 men, diet records were only collected on roughly 5% of participants. That means the 10% cap on saturated fat that continues to restrict our diet today was largely based on data from around 500 people.
The “Core Trials”: The 67,000-Person Test
Keys’s study was observational, meaning it cannot demonstrate cause-and-effect. Yet, the study was enormously influential, including becoming the foundation of our Dietary Guidelines to this day.
In the 1960s and 1970s, governments around the world recognized that observational studies, like the Seven Countries study, were insufficient. Consequently, they funded a series of large randomized controlled trials to settle the debate once and for all.
Collectively, these “core trials” tested the diet-heart hypothesis on roughly 67,000 people. The trials lasted between one and seven years and compared standard saturated fat intake (12–18.3% of calories) against a diet where saturated fat was replaced with polyunsaturated vegetable oils. The endpoints were not just cholesterol levels, but the hard outcomes that matter: heart attacks and death.
The result?
The totality of these trials did not support the hypothesis. Reducing saturated fat did not stop deaths from heart disease.
The Buried Evidence
Even worse, two of the most rigorous studies that showed harm from replacing saturated fat with vegetable oils were effectively buried for decades.
The Minnesota Coronary Experiment (1968–1973): This was the largest double-blind randomized control trial of its kind, involving over 9,000 institutionalized patients. For decades, the full results were unpublished.
In 2011, researcher Dr. Christopher Ramsden from the NIH tracked down the son of the lead investigator, Dr. Ivan Frantz. The son searched his childhood home and found the raw data on ancient magnetic computer tapes hidden in an old cardboard box in the basement.
When Ramsden analyzed this recovered data, the results were shocking: while the vegetable oil group did lower their cholesterol, for every 30 mg/dL drop in serum cholesterol, there was a 22% higher risk of death.The Sydney Diet Heart Study (1966–1973): In 2013, Ramsden also resurrected data from the Sydney study, which tested replacing saturated fat with linoleic acid (safflower oil). The results showed that the group consuming the vegetable oil had a significantly higher risk of death from coronary heart disease compared to those eating saturated fat.
These studies were not “outliers”; they were the gold standard. Yet, they were left to gather dust while Americans were told to swap butter for margarine. It might be a coincidence, but the Minnesota Coronary Experiment was co-led by Ancel Keys.
The Voices of Dissent (And the Senator Who Ignored Them)
While Keys provided the diet-heart hypothesis, it was a senate committee that turned it into law.
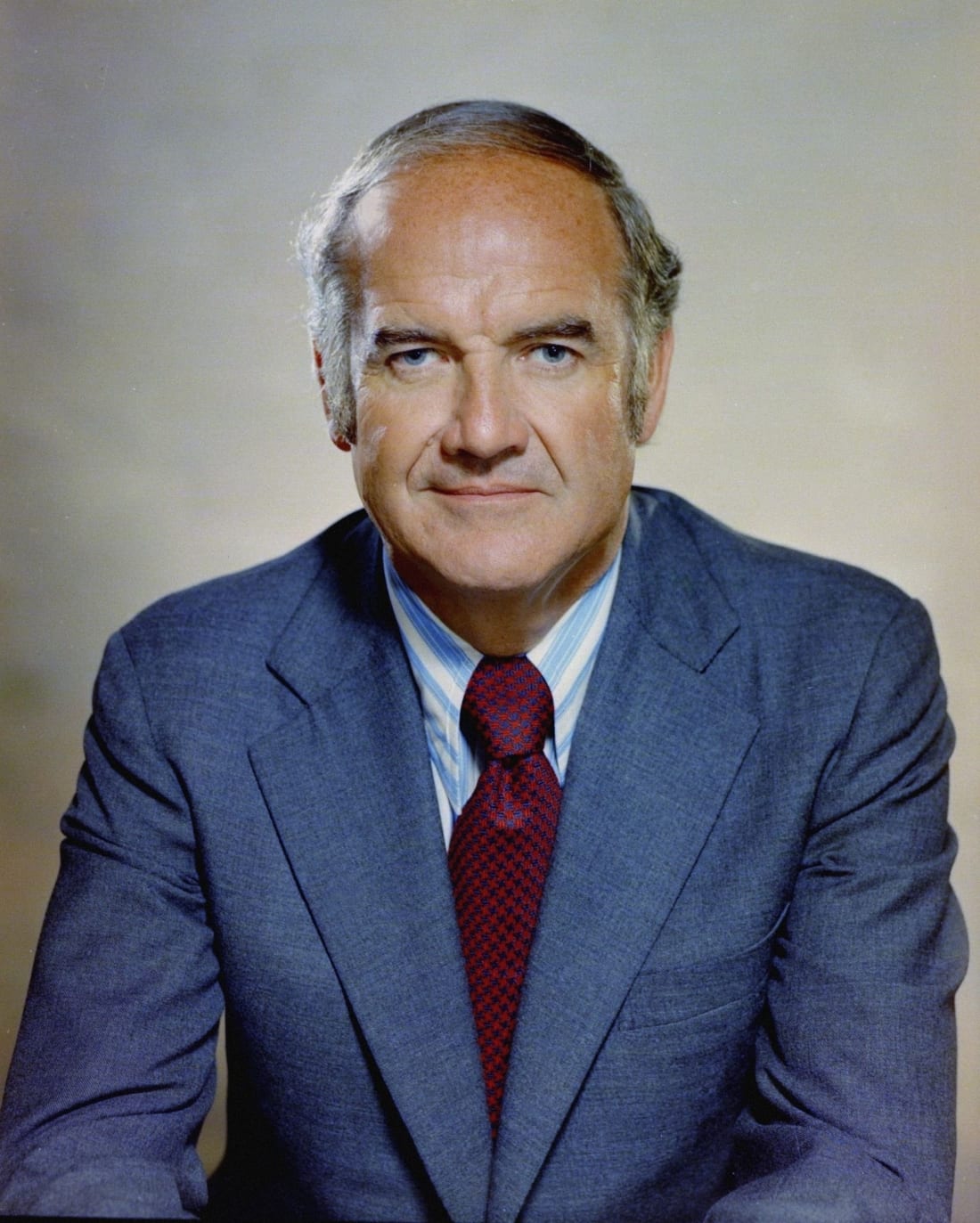
In 1977, Senator George McGovern released the “Dietary Goals for the United States.” This document was the first to explicitly set the arbitrary cap of 10% saturated fat – a number chosen not because of irrefutable proof, but because the committee felt they needed to give the public a clear, actionable target, even if the science didn’t exist to back it up.
Critics at the time were vocal, warning the government that the science was not ready. During the 1977 Senate Select Committee meeting that birthed these guidelines, the experts spoke clearly:
Dr. Robert Levy, Director of the NIH, admitted on the record that scientists did not know if cholesterol decreases the risk of heart attack: “That is still presumptive. It is unproven. There is no doubt that cholesterol can be lowered by diet…The problem with all these trials is that none of them have showed a difference in heart attack or death rate in the treated group”. He added, “Where doubt exists, as a scientific question, is whether specific lowering of cholesterol, changing the amount of saturated fat in the diet of the average American will prevent heart attack”.
Dr. Pete Ahrens, a clinical nutrition researcher, bluntly stated, “The proof is not there yet.”
Dr. Robert Olson of St. Louis University pleaded with the committee: “I pleaded in my report and will plead again orally here for more research on the problem before we make announcements to the American public”.
But politics did not wait for science. Senator McGovern, the committee chair, famously retorted to Dr. Olson: “Senators don’t have the luxury that the research scientist does of waiting until every last shred of evidence is in.”
The Truth Existed from the Beginning
The evidence to debunk the diet-heart hypothesis existed from the start and has grown stronger over time.
A 2015 study reviewed the randomized controlled trials that were available to the government committee at the exact moment they chose the saturated fat cap. The trials demonstrated that the interventions successfully lowered cholesterol, however, there was no significant difference in heart disease deaths or all-cause mortality between people consuming vegetable oils and those consuming saturated fats.
The study’s conclusion was damning: “The present review concludes that dietary advice not merely needs review; it should not have been introduced.”
Since 1957, over 350,000 people have been observed in epidemiological or observational studies to test the saturated fat hypothesis. Overwhelmingly, these studies concluded that saturated fat does not increase the risk of heart disease.
Likewise, in the last decade, nearly 20 papers reviewed all the data on saturated fat and heart disease and concluded there was insufficient evidence to support continuing to recommend the saturated fat cap.
Understanding Your Numbers: Empowerment in the Doctor’s Office
This evolved understanding is incredibly empowering for patients. For years, we focused myopically on lowering total cholesterol, or LDL, at all costs. Today, we understand biochemistry with far more nuance.
When you switch to a “Real Food” diet rich in natural fats, like the new DGA’s recommend, your lipid panel might change, but often in ways that signal better metabolic health:
HDL (The “Good” Cholesterol): Saturated fat intake can increase high-density lipoprotein (HDL) cholesterol, improving your total-to-HDL ratio, which is a better marker of cardiovascular disease risk than total cholesterol alone.
Particle Size Matters: While saturated fats can raise LDL, this increase often reflects higher levels of large LDL particles. It is the small, dense LDL particles, often driven by refined carbohydrates and sugar, that are more strongly associated with heart disease risk.
The Stroke Connection: Saturated fat intake has been associated with a decreased risk of stroke, a protective benefit that the narrow war on cholesterol ignored.
The Path Forward
The new DGA’s have done something monumental: they have validated the move away from ultra-processed factory foods and cleared the path for Americans to return to the kitchen.
The discrepancy regarding saturated fat isn’t a wall; it’s a hurdle we can easily step over with education. We don’t need to wait for policy to catch up to physiology. By understanding that “Real Food” includes healthy natural fats, we can confidently eat the pasture-raised whole egg, drink whole milk, enjoy a 100% grass-fed steak, and nourish our families without fear.
The era of industrial food is waning. The era of metabolic empowerment is just beginning.
Dr. Sina McCullough is the author of the upcoming book Hands Off My Food: How to Defend Your Food, Health, and Freedom, launching in February 2026. She holds a PhD in Nutrition and is a recognized expert in disease reversal and functional medicine. As the creator of the “Go Wild“ disease reversal program and co-host of the Beyond Labels podcast alongside farmer Joel Salatin, she is dedicated to helping people reclaim their health and freedom.
Thank you for subscribing to The MAHA Report
You can follow us at: TheMAHA_Report on X
You can also follow us at: MAHA Action on Facebook
Make America Healthy Again™ and MAHA™ are trademarks owned by MAHA TM LLC