Email
The Connection: Worsening Medical Debt; Paperwork Barriers to Coverage; Work Requirements’ Impact on Hospitals; and More
| From | The Commonwealth Fund <[email protected]> |
| Subject | The Connection: Worsening Medical Debt; Paperwork Barriers to Coverage; Work Requirements’ Impact on Hospitals; and More |
| Date | September 22, 2025 6:53 PM |
Links have been removed from this email. Learn more in the FAQ.
Links have been removed from this email. Learn more in the FAQ.
The Connection
A roundup of recent Fund publications, charts, multimedia, and other timely content.
Having trouble viewing this email? View online
September 22, 2025
Facebook ([link removed] )
LinkedIn ([link removed] )
Coverage May Vanish, but Medical Bills Will Remain
The budget reconciliation law, together with new federal regulations and expiring enhanced premium tax credits for marketplace plans, will exacerbate the medical debt problem in America. These changes create challenges for patients and providers, say Georgetown University’s Maanasa Kona and colleagues. Writing on To the Point, they propose ways that states can streamline screening processes for patients seeking financial assistance. And they suggest strategies states can use to protect patients from harmful practices, like requiring debt collectors to offer income-based payment plans.
READ MORE ([link removed] )
New Paperwork Burdens Will Harm Coverage
Millions of Americans are likely to lose their health insurance following recent Trump administration policy changes. Much of this loss of coverage will be driven by intentional inefficiencies and administrative burdens that make it more difficult for people to enroll in and maintain marketplace coverage, say analysts Jalisa Clark, Justin Giovannelli, and Christine Monahan. Writing on To the Point, they say these administrative roadblocks will hinder access to affordable insurance for current and potential marketplace customers, with immigrants and people of color experiencing the greatest impacts.
READ MORE ([link removed] )
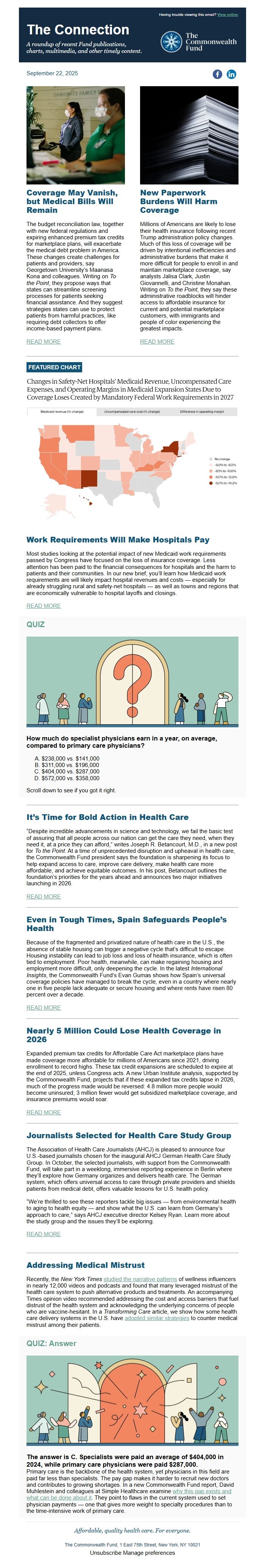
FEATURED CHART
Work Requirements Will Make Hospitals Pay
Most studies looking at the potential impact of new Medicaid work requirements passed by Congress have focused on the loss of insurance coverage. Less attention has been paid to the financial consequences for hospitals and the harm to patients and their communities. In our new brief, you’ll learn how Medicaid work requirements are will likely impact hospital revenues and costs — especially for already struggling rural and safety-net hospitals — as well as towns and regions that are economically vulnerable to hospital layoffs and closings.
READ MORE ([link removed] )
QUIZ
How much do specialist physicians earn in a year, on average, compared to primary care physicians?
- $238,000 vs. $141,000
- $311,000 vs. $196,000
- $404,000 vs. $287,000
- $572,000 vs. $358,000
Scroll down to see if you got it right.
It’s Time for Bold Action in Health Care
“Despite incredible advancements in science and technology, we fail the basic test of assuring that all people across our nation can get the care they need, when they need it, at a price they can afford,” writes Joseph R. Betancourt, M.D., in a new post for To the Point. At a time of unprecedented disruption and upheaval in health care, the Commonwealth Fund president says the foundation is sharpening its focus to help expand access to care, improve care delivery, make health care more affordable, and achieve equitable outcomes. In his post, Betancourt outlines the foundation’s priorities for the years ahead and announces two major initiatives launching in 2026.
READ MORE ([link removed] )
Even in Tough Times, Spain Safeguards People’s Health
Because of the fragmented and privatized nature of health care in the U.S., the absence of stable housing can trigger a negative cycle that’s difficult to escape. Housing instability can lead to job loss and loss of health insurance, which is often tied to employment. Poor health, meanwhile, can make regaining housing and employment more difficult, only deepening the cycle. In the latest International Insights, the Commonwealth Fund’s Evan Gumas shows how Spain’s universal coverage policies have managed to break the cycle, even in a country where nearly one in five people lack adequate or secure housing and where rents have risen 80 percent over a decade.
READ MORE ([link removed] )
Nearly 5 Million Could Lose Health Coverage in 2026
Expanded premium tax credits for Affordable Care Act marketplace plans have made coverage more affordable for millions of Americans since 2021, driving enrollment to record highs. These tax credit expansions are scheduled to expire at the end of 2025, unless Congress acts. A new Urban Institute analysis, supported by the Commonwealth Fund, projects that if these expanded tax credits lapse in 2026, much of the progress made would be reversed: 4.8 million more people would become uninsured, 3 million fewer would get subsidized marketplace coverage, and insurance premiums would soar.
READ MORE ([link removed] )
Journalists Selected for Health Care Study Group
The Association of Health Care Journalists (AHCJ) is pleased to announce four U.S.-based journalists chosen for the inaugural AHCJ German Health Care Study Group. In October, the selected journalists, with support from the Commonwealth Fund, will take part in a weeklong, immersive reporting experience in Berlin where they’ll explore how Germany organizes and delivers health care. The German system, which offers universal access to care through private providers and shields patients from medical debt, offers valuable lessons for U.S. health policy.
“We’re thrilled to see these reporters tackle big issues — from environmental health to aging to health equity — and show what the U.S. can learn from Germany’s approach to care,” says AHCJ executive director Kelsey Ryan. Learn more about the study group and the issues they’ll be exploring.
READ MORE ([link removed] )
Addressing Medical Mistrust
Recently, the New York Times studied the narrative patterns ([link removed] ) of wellness influencers in nearly 12,000 videos and podcasts and found that many leveraged mistrust of the health care system to push alternative products and treatments. An accompanying Times opinion video recommended addressing the cost and access barriers that fuel distrust of the health system and acknowledging the underlying concerns of people who are vaccine-hesitant. In a Transforming Care article, we show how some health care delivery systems in the U.S. have adopted similar strategies ([link removed] ) to counter medical mistrust among their patients.
QUIZ: Answer
The answer is C. Specialists were paid an average of $404,000 in 2024, while primary care physicians were paid $287,000.
Primary care is the backbone of the health system, yet physicians in this field are paid far less than specialists. The pay gap makes it harder to recruit new doctors and contributes to growing shortages. In a new Commonwealth Fund report, David Muhlestein and colleagues at Simple Healthcare examine why this gap exists and what can be done about it ([link removed] ) . They point to flaws in the current system used to set physician payments — one that gives more weight to specialty procedures than to the time-intensive work of primary care.
Affordable, quality health care. For everyone.
The Commonwealth Fund, 1 East 75th Street, New York, NY 10021
Unsubscribe ([link removed] )
Manage preferences ([link removed] )
A roundup of recent Fund publications, charts, multimedia, and other timely content.
Having trouble viewing this email? View online
September 22, 2025
Facebook ([link removed] )
LinkedIn ([link removed] )
Coverage May Vanish, but Medical Bills Will Remain
The budget reconciliation law, together with new federal regulations and expiring enhanced premium tax credits for marketplace plans, will exacerbate the medical debt problem in America. These changes create challenges for patients and providers, say Georgetown University’s Maanasa Kona and colleagues. Writing on To the Point, they propose ways that states can streamline screening processes for patients seeking financial assistance. And they suggest strategies states can use to protect patients from harmful practices, like requiring debt collectors to offer income-based payment plans.
READ MORE ([link removed] )
New Paperwork Burdens Will Harm Coverage
Millions of Americans are likely to lose their health insurance following recent Trump administration policy changes. Much of this loss of coverage will be driven by intentional inefficiencies and administrative burdens that make it more difficult for people to enroll in and maintain marketplace coverage, say analysts Jalisa Clark, Justin Giovannelli, and Christine Monahan. Writing on To the Point, they say these administrative roadblocks will hinder access to affordable insurance for current and potential marketplace customers, with immigrants and people of color experiencing the greatest impacts.
READ MORE ([link removed] )
FEATURED CHART
Work Requirements Will Make Hospitals Pay
Most studies looking at the potential impact of new Medicaid work requirements passed by Congress have focused on the loss of insurance coverage. Less attention has been paid to the financial consequences for hospitals and the harm to patients and their communities. In our new brief, you’ll learn how Medicaid work requirements are will likely impact hospital revenues and costs — especially for already struggling rural and safety-net hospitals — as well as towns and regions that are economically vulnerable to hospital layoffs and closings.
READ MORE ([link removed] )
QUIZ
How much do specialist physicians earn in a year, on average, compared to primary care physicians?
- $238,000 vs. $141,000
- $311,000 vs. $196,000
- $404,000 vs. $287,000
- $572,000 vs. $358,000
Scroll down to see if you got it right.
It’s Time for Bold Action in Health Care
“Despite incredible advancements in science and technology, we fail the basic test of assuring that all people across our nation can get the care they need, when they need it, at a price they can afford,” writes Joseph R. Betancourt, M.D., in a new post for To the Point. At a time of unprecedented disruption and upheaval in health care, the Commonwealth Fund president says the foundation is sharpening its focus to help expand access to care, improve care delivery, make health care more affordable, and achieve equitable outcomes. In his post, Betancourt outlines the foundation’s priorities for the years ahead and announces two major initiatives launching in 2026.
READ MORE ([link removed] )
Even in Tough Times, Spain Safeguards People’s Health
Because of the fragmented and privatized nature of health care in the U.S., the absence of stable housing can trigger a negative cycle that’s difficult to escape. Housing instability can lead to job loss and loss of health insurance, which is often tied to employment. Poor health, meanwhile, can make regaining housing and employment more difficult, only deepening the cycle. In the latest International Insights, the Commonwealth Fund’s Evan Gumas shows how Spain’s universal coverage policies have managed to break the cycle, even in a country where nearly one in five people lack adequate or secure housing and where rents have risen 80 percent over a decade.
READ MORE ([link removed] )
Nearly 5 Million Could Lose Health Coverage in 2026
Expanded premium tax credits for Affordable Care Act marketplace plans have made coverage more affordable for millions of Americans since 2021, driving enrollment to record highs. These tax credit expansions are scheduled to expire at the end of 2025, unless Congress acts. A new Urban Institute analysis, supported by the Commonwealth Fund, projects that if these expanded tax credits lapse in 2026, much of the progress made would be reversed: 4.8 million more people would become uninsured, 3 million fewer would get subsidized marketplace coverage, and insurance premiums would soar.
READ MORE ([link removed] )
Journalists Selected for Health Care Study Group
The Association of Health Care Journalists (AHCJ) is pleased to announce four U.S.-based journalists chosen for the inaugural AHCJ German Health Care Study Group. In October, the selected journalists, with support from the Commonwealth Fund, will take part in a weeklong, immersive reporting experience in Berlin where they’ll explore how Germany organizes and delivers health care. The German system, which offers universal access to care through private providers and shields patients from medical debt, offers valuable lessons for U.S. health policy.
“We’re thrilled to see these reporters tackle big issues — from environmental health to aging to health equity — and show what the U.S. can learn from Germany’s approach to care,” says AHCJ executive director Kelsey Ryan. Learn more about the study group and the issues they’ll be exploring.
READ MORE ([link removed] )
Addressing Medical Mistrust
Recently, the New York Times studied the narrative patterns ([link removed] ) of wellness influencers in nearly 12,000 videos and podcasts and found that many leveraged mistrust of the health care system to push alternative products and treatments. An accompanying Times opinion video recommended addressing the cost and access barriers that fuel distrust of the health system and acknowledging the underlying concerns of people who are vaccine-hesitant. In a Transforming Care article, we show how some health care delivery systems in the U.S. have adopted similar strategies ([link removed] ) to counter medical mistrust among their patients.
QUIZ: Answer
The answer is C. Specialists were paid an average of $404,000 in 2024, while primary care physicians were paid $287,000.
Primary care is the backbone of the health system, yet physicians in this field are paid far less than specialists. The pay gap makes it harder to recruit new doctors and contributes to growing shortages. In a new Commonwealth Fund report, David Muhlestein and colleagues at Simple Healthcare examine why this gap exists and what can be done about it ([link removed] ) . They point to flaws in the current system used to set physician payments — one that gives more weight to specialty procedures than to the time-intensive work of primary care.
Affordable, quality health care. For everyone.
The Commonwealth Fund, 1 East 75th Street, New York, NY 10021
Unsubscribe ([link removed] )
Manage preferences ([link removed] )
Message Analysis
- Sender: Commonwealth Fund
- Political Party: n/a
- Country: United States
- State/Locality: n/a
- Office: n/a
