Email
The Connection: A Look at U.S. Maternal Deaths; When Insurers Deny Claims; 340B Drug Program Explained; and More
| From | The Commonwealth Fund <[email protected]> |
| Subject | The Connection: A Look at U.S. Maternal Deaths; When Insurers Deny Claims; 340B Drug Program Explained; and More |
| Date | August 11, 2025 7:00 PM |
Links have been removed from this email. Learn more in the FAQ.
Links have been removed from this email. Learn more in the FAQ.
The Connection
A roundup of recent Fund publications, charts, multimedia, and other timely content.
Having trouble viewing this email? View online
August 11, 2025
Facebook ([link removed] )
LinkedIn ([link removed] )
What’s Driving Maternal Deaths in the U.S.?
The United States has long had the highest maternal mortality rate of any wealthy nation — a rate that peaked in 2021, during the COVID-19 pandemic. In analyzing the latest national data on maternal mortality, a new Commonwealth Fund report offers a broad look at the causes and characteristics of preventable maternal deaths, including sharp differences linked to race and geography. While maternal mortality has nearly returned to prepandemic levels, the outlook remains troubling, as federal budget cuts could reverse recent improvement.
READ MORE ([link removed] )
Who Suffers Most When Insurers Deny Claims?
Millions of Americans with private health insurance are denied coverage for medical services every year, often because of billing or administrative errors. While patients with the time and resources to challenge these denials usually win, new research shows the system can be stacked against patients with low income and people of color, exacerbating health care inequities. On To the Point, the University of Toronto’s Alex Hoagland looks at the causes and consequences of private health insurance claim denials, along with potential policy solutions.
READ MORE ([link removed] )
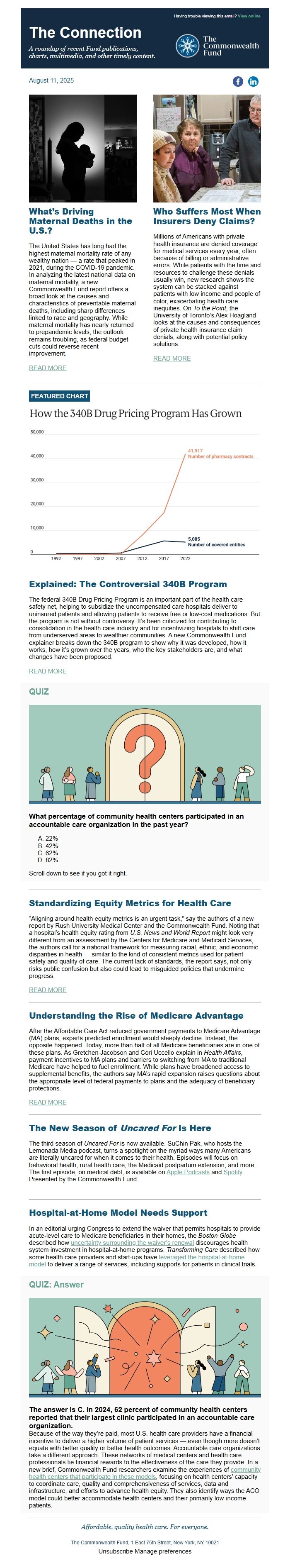
FEATURED CHART
Explained: The Controversial 340B Program
The federal 340B Drug Pricing Program is an important part of the health care safety net, helping to subsidize the uncompensated care hospitals deliver to uninsured patients and allowing patients to receive free or low-cost medications. But the program is not without controversy. It’s been criticized for contributing to consolidation in the health care industry and for incentivizing hospitals to shift care from underserved areas to wealthier communities. A new Commonwealth Fund explainer breaks down the 340B program to show why it was developed, how it works, how it’s grown over the years, who the key stakeholders are, and what changes have been proposed.
READ MORE ([link removed] )
QUIZ
What percentage of community health centers participated in an accountable care organization in the past year?
- 22%
- 42%
- 62%
- 82%
Scroll down to see if you got it right.
Standardizing Equity Metrics for Health Care
“Aligning around health equity metrics is an urgent task,” say the authors of a new report by Rush University Medical Center and the Commonwealth Fund. Noting that a hospital’s health equity rating from U.S. News and World Report might look very different from an assessment by the Centers for Medicare and Medicaid Services, the authors call for a national framework for measuring racial, ethnic, and economic disparities in health — similar to the kind of consistent metrics used for patient safety and quality of care. The current lack of standards, the report says, not only risks public confusion but also could lead to misguided policies that undermine progress.
READ MORE ([link removed] )
Understanding the Rise of Medicare Advantage
After the Affordable Care Act reduced government payments to Medicare Advantage (MA) plans, experts predicted enrollment would steeply decline. Instead, the opposite happened. Today, more than half of all Medicare beneficiaries are in one of these plans. As Gretchen Jacobson and Cori Uccello explain in Health Affairs, payment incentives to MA plans and barriers to switching from MA to traditional Medicare have helped to fuel enrollment. While plans have broadened access to supplemental benefits, the authors say MA’s rapid expansion raises questions about the appropriate level of federal payments to plans and the adequacy of beneficiary protections.
READ MORE ([link removed] )
The New Season of Uncared For Is Here
The third season of Uncared For is now available. SuChin Pak, who hosts the Lemonada Media podcast, turns a spotlight on the myriad ways many Americans are literally uncared for when it comes to their health. Episodes will focus on behavioral health, rural health care, the Medicaid postpartum extension, and more. The first episode, on medical debt, is available on Apple Podcasts ([link removed] ) and Spotify ([link removed] ) . Presented by the Commonwealth Fund.
Hospital-at-Home Model Needs Support
In an editorial urging Congress to extend the waiver that permits hospitals to provide acute-level care to Medicare beneficiaries in their homes, the Boston Globe described how uncertainty surrounding the waiver’s renewal ([link removed] ) discourages health system investment in hospital-at-home programs. Transforming Care described how some health care providers and start-ups have leveraged the hospital-at-home model ([link removed] ) to deliver a range of services, including supports for patients in clinical trials.
QUIZ: Answer
The answer is C. In 2024, 62 percent of community health centers reported that their largest clinic participated in an accountable care organization.
Because of the way they’re paid, most U.S. health care providers have a financial incentive to deliver a higher volume of patient services — even though more doesn’t equate with better quality or better health outcomes. Accountable care organizations take a different approach. These networks of medical centers and health care professionals tie financial rewards to the effectiveness of the care they provide. In a new brief, Commonwealth Fund researchers examine the experiences of community health centers that participate in these models ([link removed] ) , focusing on health centers’ capacity to coordinate care, quality and comprehensiveness of services, data and infrastructure, and efforts to advance health equity. They also identify ways the ACO model could better accommodate health centers and their primarily low-income patients.
Affordable, quality health care. For everyone.
The Commonwealth Fund, 1 East 75th Street, New York, NY 10021
Unsubscribe ([link removed] )
Manage preferences ([link removed] )
A roundup of recent Fund publications, charts, multimedia, and other timely content.
Having trouble viewing this email? View online
August 11, 2025
Facebook ([link removed] )
LinkedIn ([link removed] )
What’s Driving Maternal Deaths in the U.S.?
The United States has long had the highest maternal mortality rate of any wealthy nation — a rate that peaked in 2021, during the COVID-19 pandemic. In analyzing the latest national data on maternal mortality, a new Commonwealth Fund report offers a broad look at the causes and characteristics of preventable maternal deaths, including sharp differences linked to race and geography. While maternal mortality has nearly returned to prepandemic levels, the outlook remains troubling, as federal budget cuts could reverse recent improvement.
READ MORE ([link removed] )
Who Suffers Most When Insurers Deny Claims?
Millions of Americans with private health insurance are denied coverage for medical services every year, often because of billing or administrative errors. While patients with the time and resources to challenge these denials usually win, new research shows the system can be stacked against patients with low income and people of color, exacerbating health care inequities. On To the Point, the University of Toronto’s Alex Hoagland looks at the causes and consequences of private health insurance claim denials, along with potential policy solutions.
READ MORE ([link removed] )
FEATURED CHART
Explained: The Controversial 340B Program
The federal 340B Drug Pricing Program is an important part of the health care safety net, helping to subsidize the uncompensated care hospitals deliver to uninsured patients and allowing patients to receive free or low-cost medications. But the program is not without controversy. It’s been criticized for contributing to consolidation in the health care industry and for incentivizing hospitals to shift care from underserved areas to wealthier communities. A new Commonwealth Fund explainer breaks down the 340B program to show why it was developed, how it works, how it’s grown over the years, who the key stakeholders are, and what changes have been proposed.
READ MORE ([link removed] )
QUIZ
What percentage of community health centers participated in an accountable care organization in the past year?
- 22%
- 42%
- 62%
- 82%
Scroll down to see if you got it right.
Standardizing Equity Metrics for Health Care
“Aligning around health equity metrics is an urgent task,” say the authors of a new report by Rush University Medical Center and the Commonwealth Fund. Noting that a hospital’s health equity rating from U.S. News and World Report might look very different from an assessment by the Centers for Medicare and Medicaid Services, the authors call for a national framework for measuring racial, ethnic, and economic disparities in health — similar to the kind of consistent metrics used for patient safety and quality of care. The current lack of standards, the report says, not only risks public confusion but also could lead to misguided policies that undermine progress.
READ MORE ([link removed] )
Understanding the Rise of Medicare Advantage
After the Affordable Care Act reduced government payments to Medicare Advantage (MA) plans, experts predicted enrollment would steeply decline. Instead, the opposite happened. Today, more than half of all Medicare beneficiaries are in one of these plans. As Gretchen Jacobson and Cori Uccello explain in Health Affairs, payment incentives to MA plans and barriers to switching from MA to traditional Medicare have helped to fuel enrollment. While plans have broadened access to supplemental benefits, the authors say MA’s rapid expansion raises questions about the appropriate level of federal payments to plans and the adequacy of beneficiary protections.
READ MORE ([link removed] )
The New Season of Uncared For Is Here
The third season of Uncared For is now available. SuChin Pak, who hosts the Lemonada Media podcast, turns a spotlight on the myriad ways many Americans are literally uncared for when it comes to their health. Episodes will focus on behavioral health, rural health care, the Medicaid postpartum extension, and more. The first episode, on medical debt, is available on Apple Podcasts ([link removed] ) and Spotify ([link removed] ) . Presented by the Commonwealth Fund.
Hospital-at-Home Model Needs Support
In an editorial urging Congress to extend the waiver that permits hospitals to provide acute-level care to Medicare beneficiaries in their homes, the Boston Globe described how uncertainty surrounding the waiver’s renewal ([link removed] ) discourages health system investment in hospital-at-home programs. Transforming Care described how some health care providers and start-ups have leveraged the hospital-at-home model ([link removed] ) to deliver a range of services, including supports for patients in clinical trials.
QUIZ: Answer
The answer is C. In 2024, 62 percent of community health centers reported that their largest clinic participated in an accountable care organization.
Because of the way they’re paid, most U.S. health care providers have a financial incentive to deliver a higher volume of patient services — even though more doesn’t equate with better quality or better health outcomes. Accountable care organizations take a different approach. These networks of medical centers and health care professionals tie financial rewards to the effectiveness of the care they provide. In a new brief, Commonwealth Fund researchers examine the experiences of community health centers that participate in these models ([link removed] ) , focusing on health centers’ capacity to coordinate care, quality and comprehensiveness of services, data and infrastructure, and efforts to advance health equity. They also identify ways the ACO model could better accommodate health centers and their primarily low-income patients.
Affordable, quality health care. For everyone.
The Commonwealth Fund, 1 East 75th Street, New York, NY 10021
Unsubscribe ([link removed] )
Manage preferences ([link removed] )
Message Analysis
- Sender: Commonwealth Fund
- Political Party: n/a
- Country: United States
- State/Locality: n/a
- Office: n/a
